Slide 1 of 47
Editor's Comment
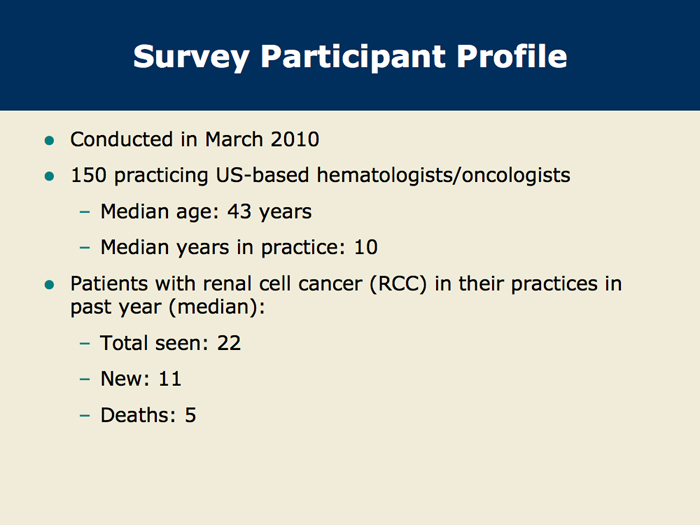
(Neil Love, MD): This March 2010 national survey of 150 US-based medical oncologists is the final part of a yearlong effort to address important CME needs in the management of renal cell cancer. The interventions in the project included three nationally distributed audio programs and three virtual video web presentations. A faculty of 12 RCC clinical investigators participated in the needs assessment, education programs and Patterns of Care studies. My editor's comments for this slide set include select results from a survey of our faculty. A printable, downloadable version of this program is available.
Slide 4 of 47
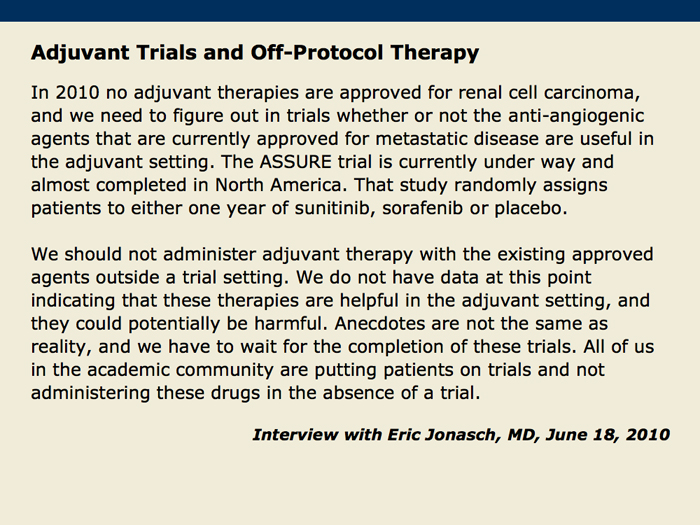
The survey focused on several issues that were identified both in the three CME activities by the faculty and in prior polls of oncologists in practice. I met with one of the faculty, Dr Eric Jonasch, on June 18, 2010 for an interview. We reviewed the major findings, and edited comments from Dr Jonasch are included on four slides of our 47-slide set.
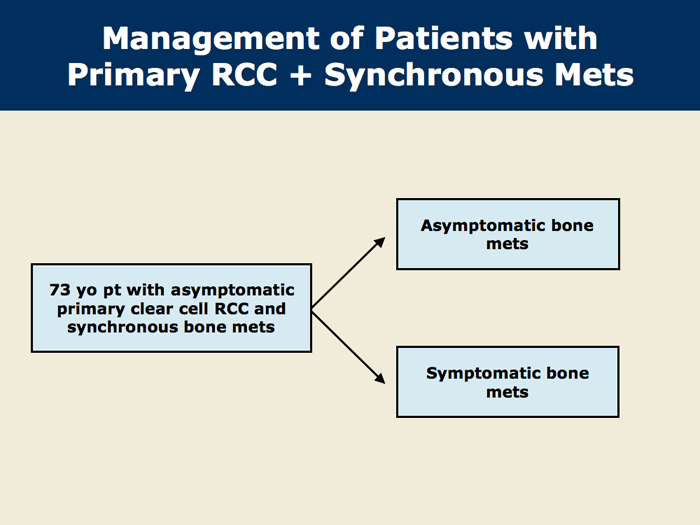
Slide 6 of 47
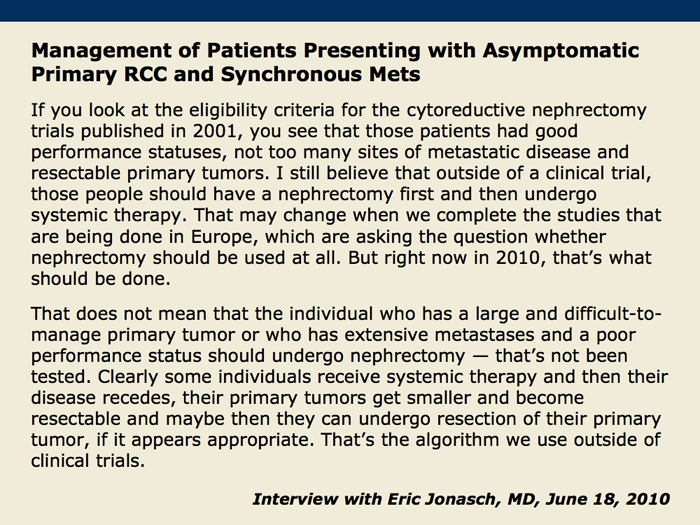
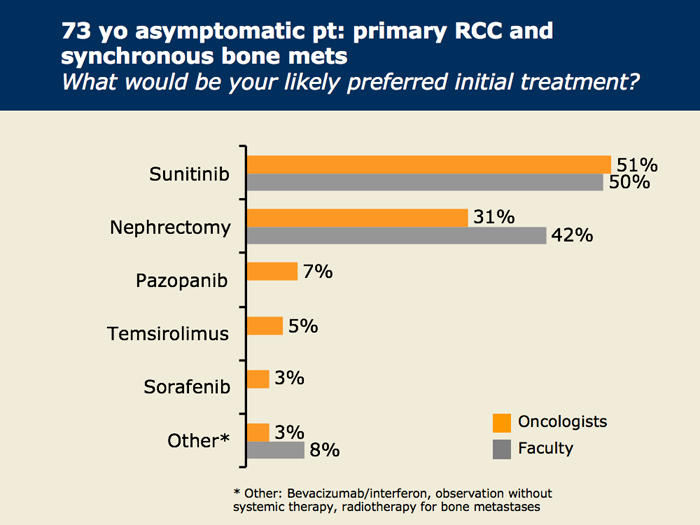
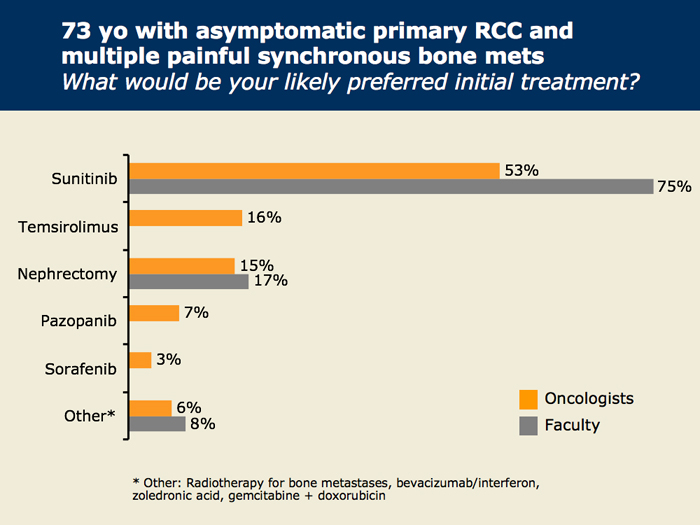
Somewhat surprisingly, the RCC issue of greatest interest to oncologists was the management approach for patients presenting with asymptomatic primary tumors and synchronous mets. We asked about two scenarios, one in which the mets were asymptomatic and the other with more extensive mets that were symptomatic.
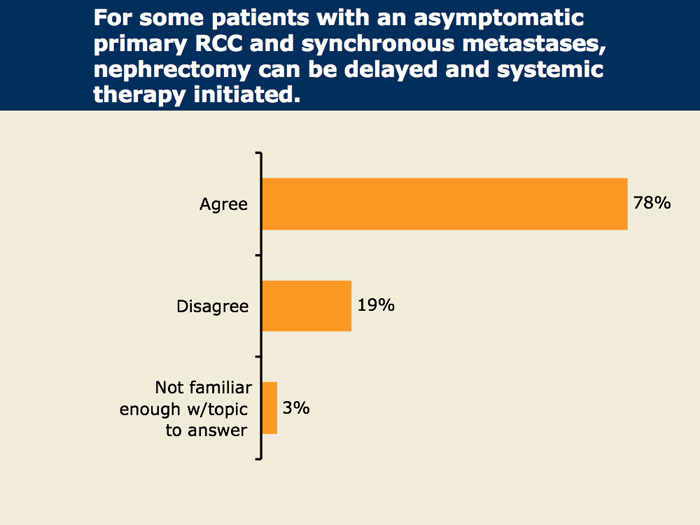
Slide 7 of 47
The management approach for patients presenting with an asymptomatic primary RCC and synchronous mets is controversial and may reflect an uncommon scenario, but 78 percent of oncologists — perhaps following a model recently integrated into the management of the analogous situation in colorectal cancer — strongly consider initial systemic therapy rather than cytoreductive nephrectomy. As will be clear, the faculty is less enthused about this practice.
Slide 10 of 47
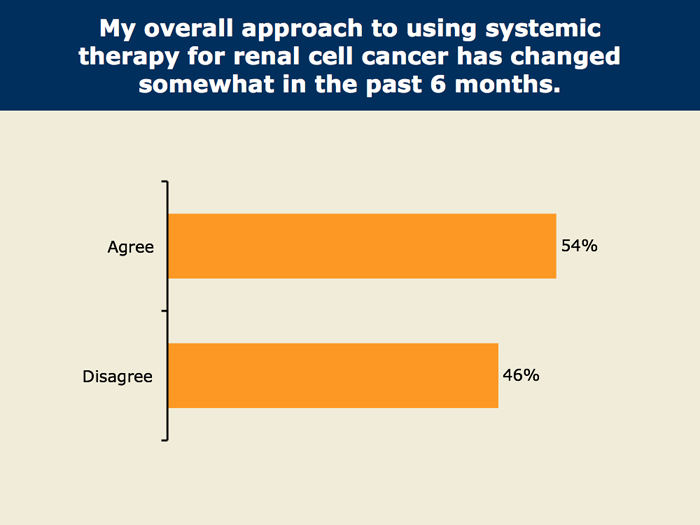
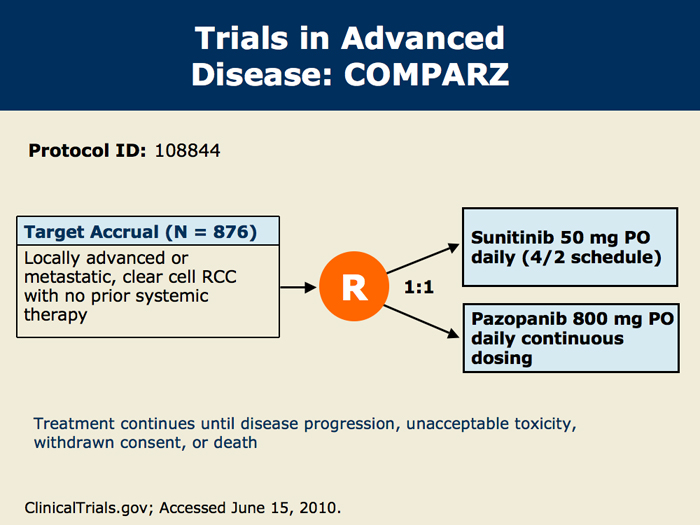
The second major CME topic relates to the selection of systemic therapy in advanced disease. There is considerable variation currently, reflecting the recent evolution of three new classes of agents that have proven helpful with the disease: TKIs, mTOR inhibitors and anti-VEGF agents such as bevacizumab.
Slide 11 of 47
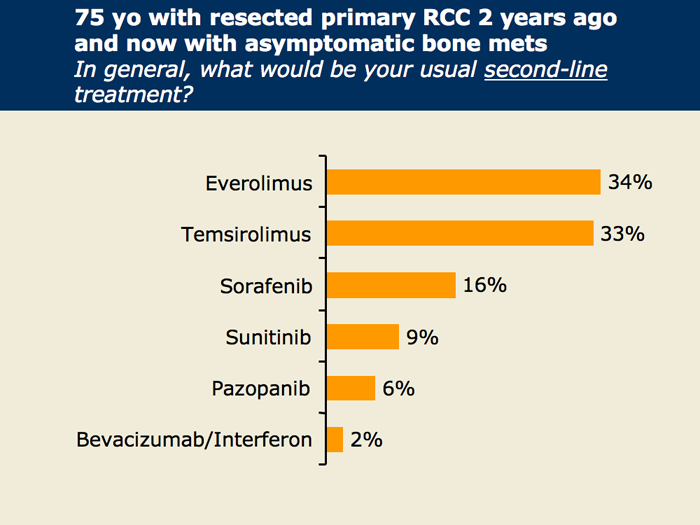
Dr Jonasch notes that in the most common scenario, in which patients do not have emergent clinical and biochemical findings, the evidence-based first-line options in his mind are sunitinib, pazopanib and bevacizumab/interferon. For first-line treatment of patients with poor-risk disease, temsirolimus has been studied the most extensively and is standard, and while there is no standard second-line treatment after TKIs, everolimus has clinical trial data supporting its use for these patients.
Slide 12 of 47
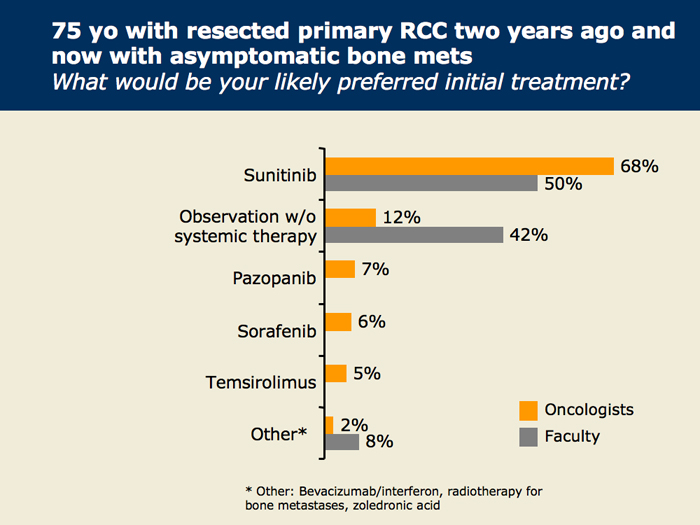
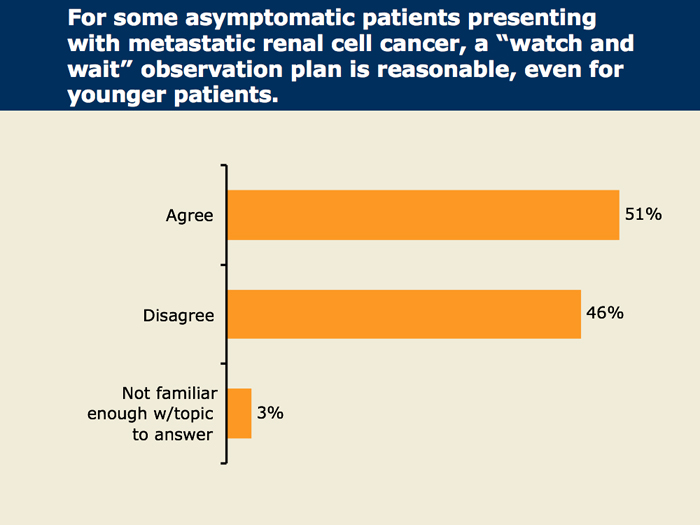
The initial education event in this initiative was a "Think Tank" co-chaired by Dr Robert Figlin. We gathered six investigators and spent the day in our recording studio in Miami planning an initial survey evaluation of our target education audience (medical oncologists) and establishing a series of major content objectives that are capsulized in our list of four. One of the faculty, Dr Michael Atkins, was particularly convinced that the strategy of expectant observation without specific treatment perhaps could be used more, but half of our oncologists don't seem to support this strategy in this situation.
Slide 13 of 47
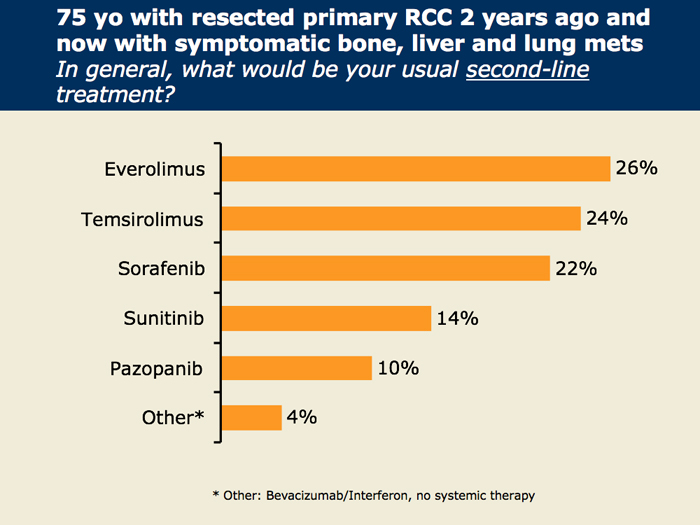
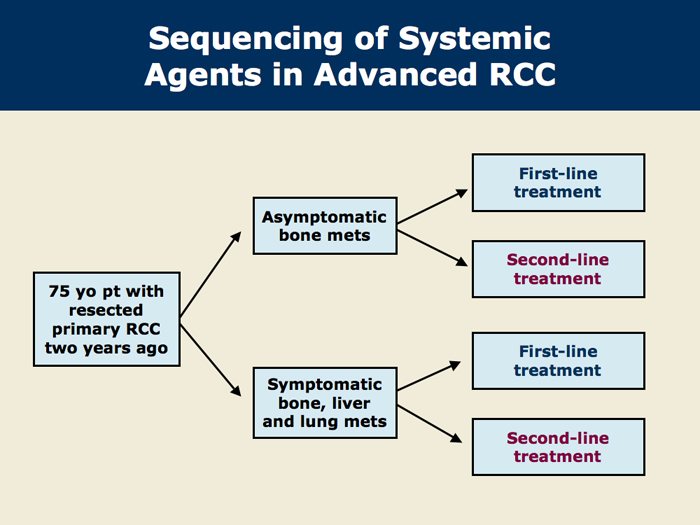
With the faculty's advice we created a series of four questions that relate to the choice and sequence of agents in advanced disease. The first scenario relates to the choice of treatment in both the first- and second-line settings for patients with asymptomatic bone mets, and the second scenario focuses on the patient with widespread symptomatic mets.
Slide 16 of 47
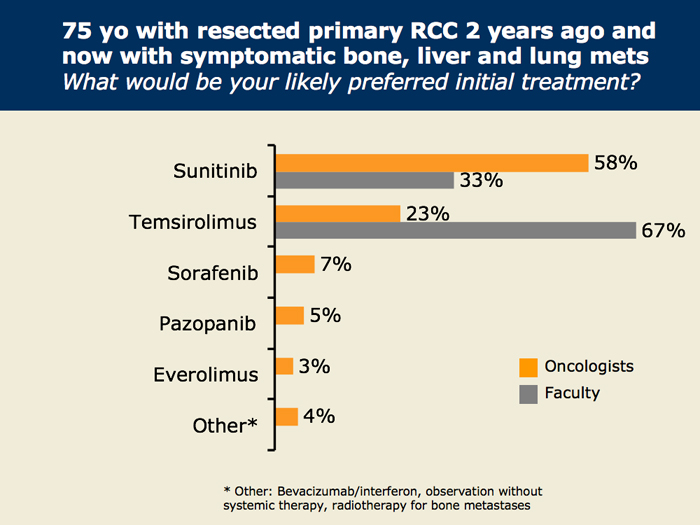
When the case is changed to state that the patient has widespread symptomatic liver, lung and bone mets, there is a noticeable increase in the use of temsirolimus among the oncologists, but sunitinib is still the most frequently chosen agent. Eight of our 12 faculty preferred to use temsirolimus as their first-line treatment.
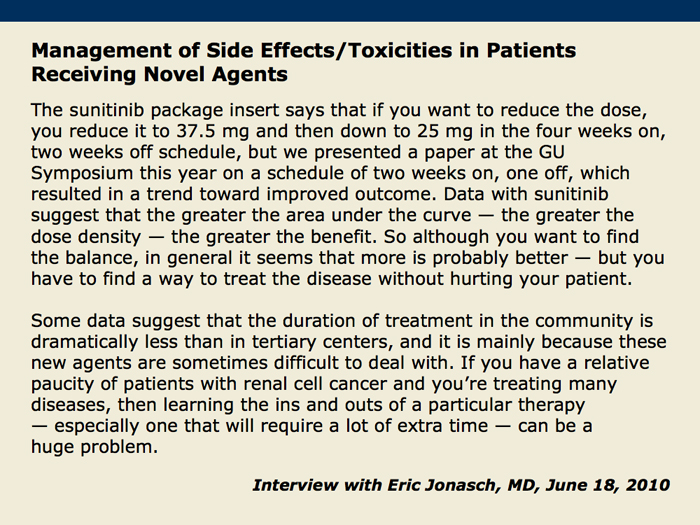
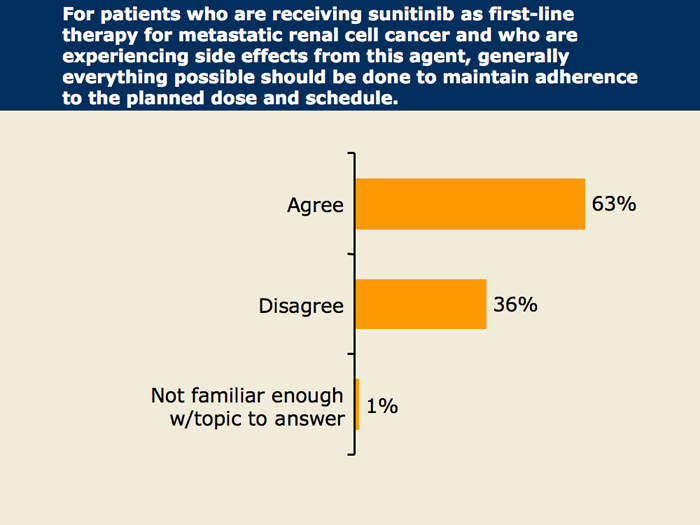
Slide 21 of 47
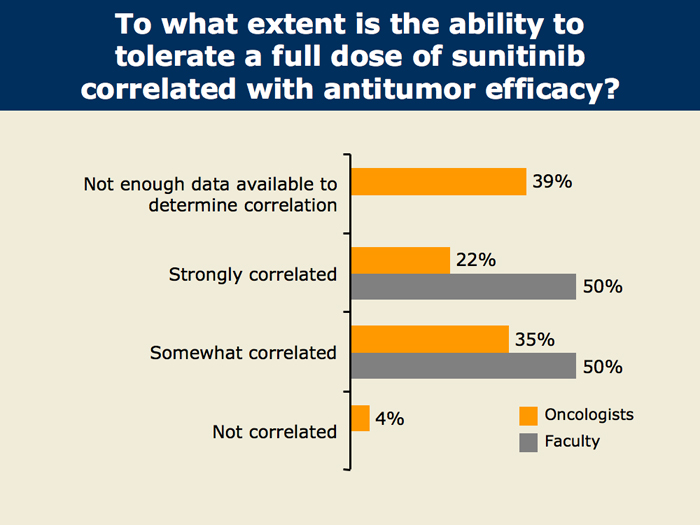
A key controversial issue in the use of these challenging agents is whether there is a significant correlation between drug dose and the duration of exposure the patient receives and treatment benefit. Only a little more than half of the practicing oncologists support a correlation of benefit with the ability to maintain a full sunitinib dose, while all of the faculty believe there is at least some correlation between dose and exposure duration and treatment benefit.
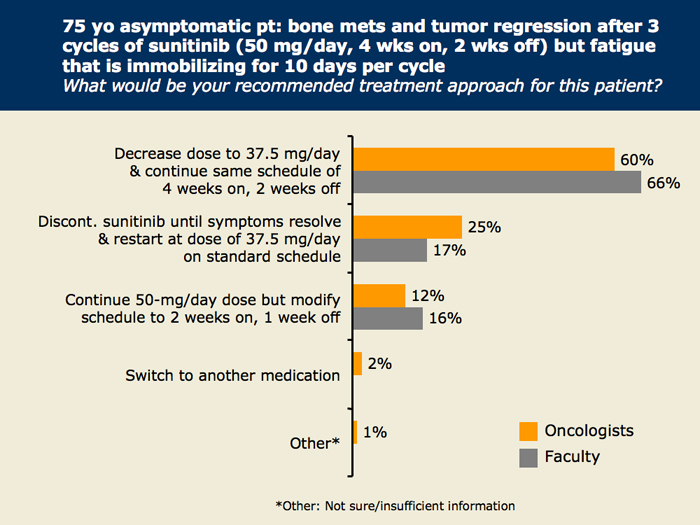
Slide 23 of 47
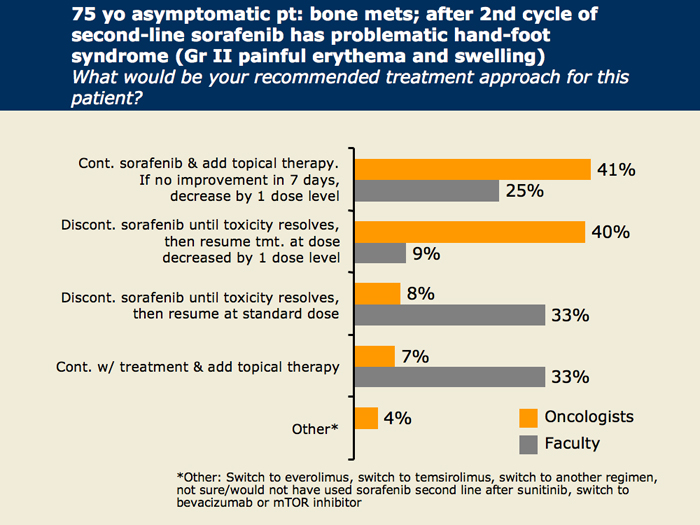
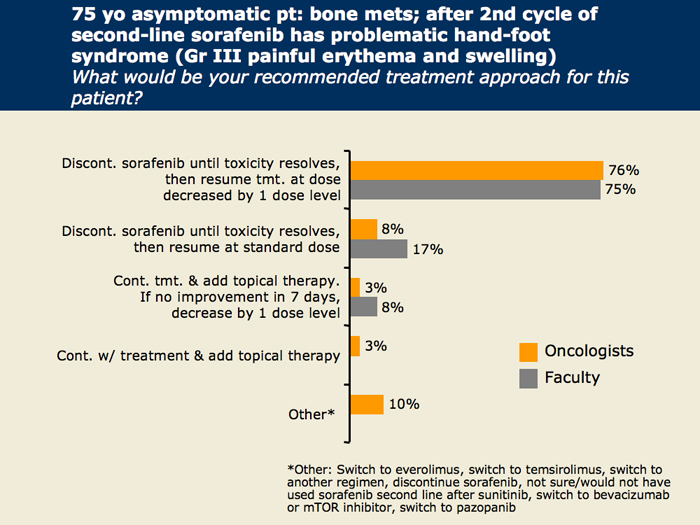
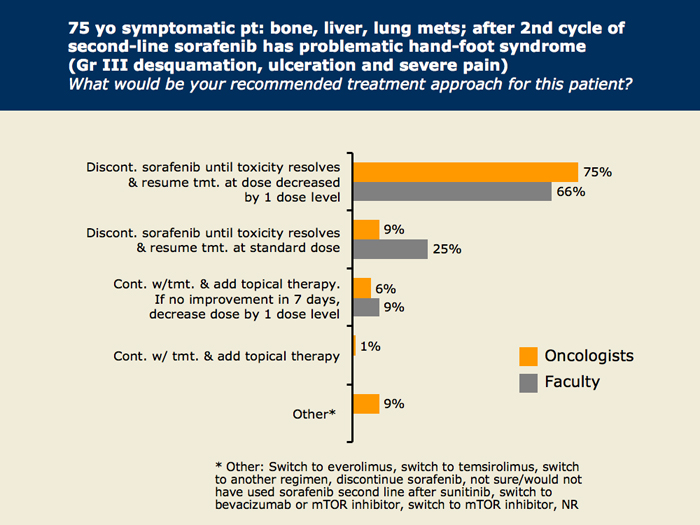
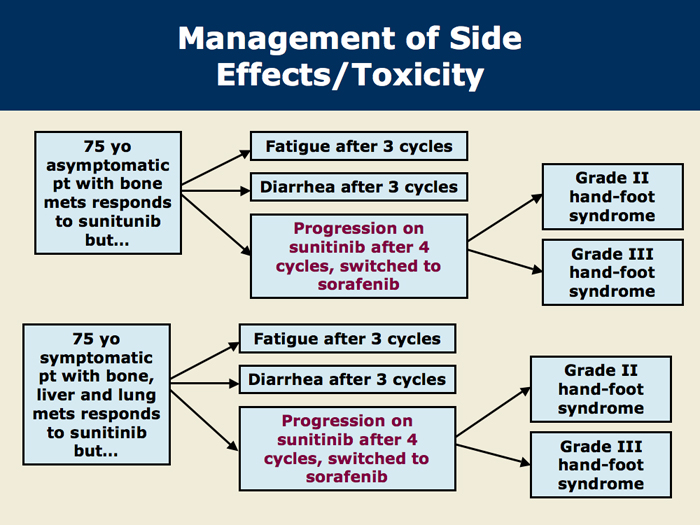
To test the clinical algorithm for 2010 in this disease, we presented two similar variants of a challenging case in which the patient has an antitumor response to sunitinib but experiences toxicity. In variant one the asymptomatic patient has bone mets but develops debilitating fatigue in one case and debilitating diarrhea in another. In the second variant the mets are more widespread and symptomatic. For both scenarios we asked about second-line therapy also.
Slide 25 of 47
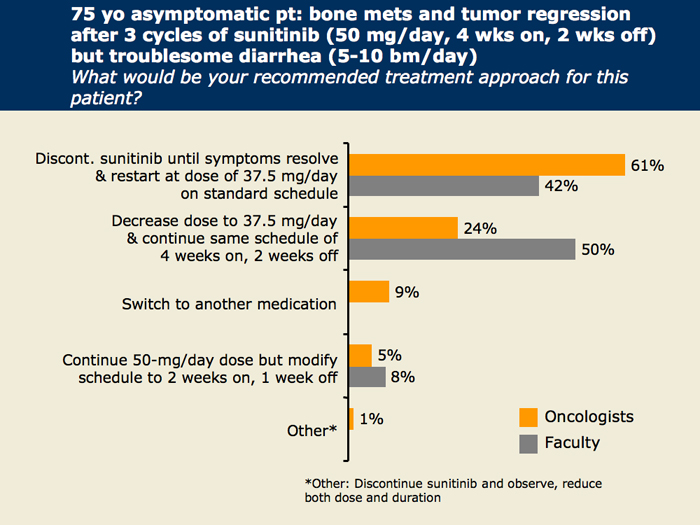
For the patient with asymptomatic bone mets and troublesome treatment-related diarrhea, the management strategy is the same for both the practicing oncologists and the faculty, and the majority recommend decreasing the next dose level after a treatment break and resolution of symptoms.
Slide 28 of 47
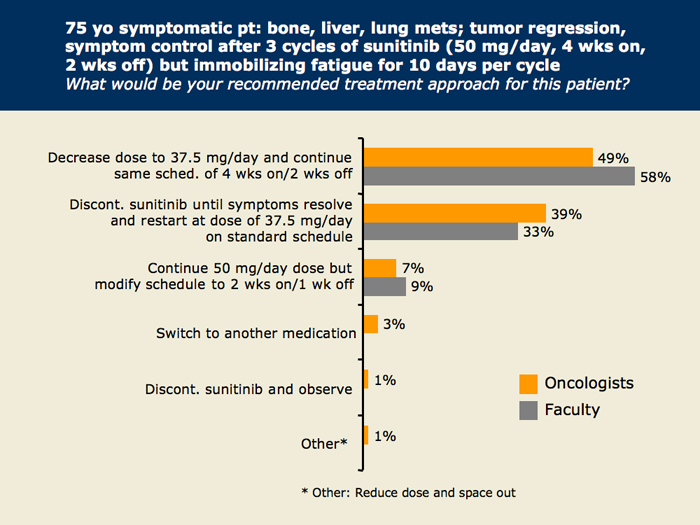
For the patient with widespread symptomatic mets and immobilizing treatment-related fatigue, similar to what was seen for the previous patient with asymptomatic bone mets, there is agreement in both groups about decreasing the next dose level, in some cases after a treatment break. The exact method used to alter the medication differs among the physicians.
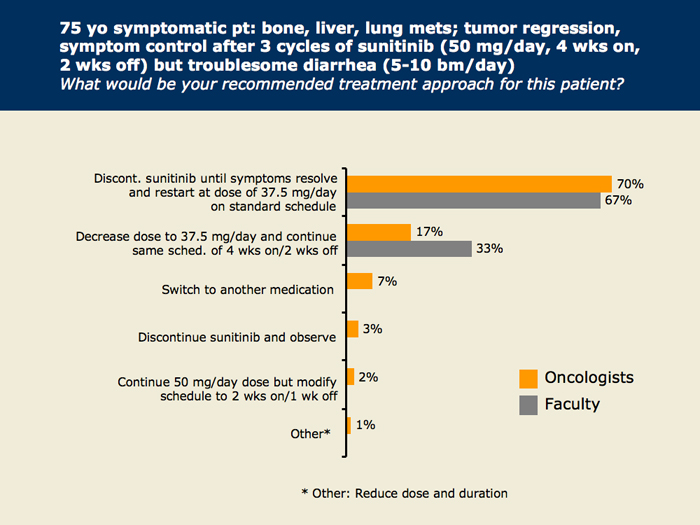
Slide 29 of 47
For the patient with widespread symptomatic mets and troublesome treatment-related diarrhea, the majority of both oncologists and faculty recommend decreasing the next dose level after a treatment break and resolution of symptoms, which is similar to what was seen for the previous patient with asymptomatic bone mets.
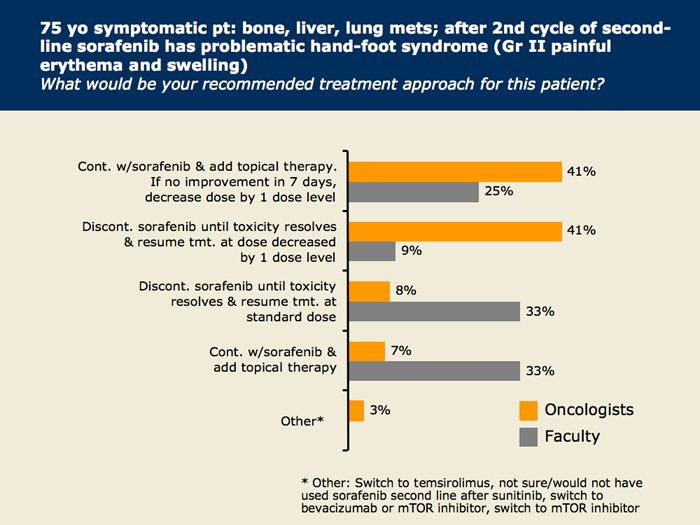
Slide 30 of 47
For the patient with widespread symptomatic mets and Grade II hand-foot syndrome on second-line sorafenib, similar to what was seen for the previous patient with asymptomatic bone mets, there is a major division about whether to hold off on therapy or not in both oncologists and faculty.
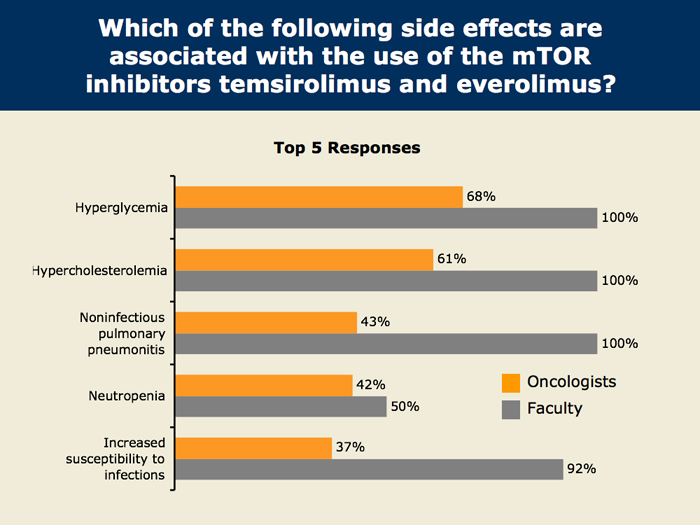
Slide 32 of 47
When we asked about the side effects associated with mTOR inhibitors, we found that four specific complications that are well known to virtually our entire faculty are not quite so well known to practicing oncologists, more than one third of whom were not aware of the association of these important complications with these agents.